
Realising the potential of food and drink in a patient’s recovery journey
In November 2022, NHS England (NHSE) published The National Standards for Healthcare food and drink¹ which once again shone a spotlight on the vital role food plays in a patient’s recovery and in the wellbeing of staff and visitors.
The standards, which followed the Independent Review of NHS Hospital Food ² in 2020, have significantly raised the focus placed on food and drink in healthcare settings, by introducing a legally binding set of requirements. Emphasising the intrinsic value of ‘food as medicine’, hospital nutrition and hydration has been elevated to a board-level concern - requiring that Trusts have a designated board member and a standing agenda item addressing compliance.
As a partner in the food standards development working group, Sodexo’s food and nutrition experts contributed to shaping the standards and we’re confident, that by working in partnership with the NHS, they will enhance the wellbeing and recovery of patients, while providing respite for staff to recuperate during their breaks.
“Developing the standards was a chance to make a real difference and look at the wider aspects of how the NHS is serving healthcare catering. So, looking at food safety, nutrition, and trying to bring services together to improve the patient recovery.”
Phil Shelley, Chair of the National Food Review
The standards are holistic and cover many of the aspects of healthcare food delivery:
- Governance, monitoring and control
- Workforce development, skills and expertise
- Food waste and the environmental impact
- Choice and quality of the offer.
Since the Independent Review of NHS Hospital food, and ahead of the publication of the National Standards, Sodexo recognised some of the challenges identified and undertook a review of the patients’ end-to-end recovery journey to, not only ensure the standards were met, but target new service innovations in the areas of biggest impact.
Learn more now: The new National Healthcare Food & Drink Standards - Interview with Phil Shelley
The importance of hospital food and drink
The impact of malnutrition and poor diet on the NHS, and its ability to treat acute and chronic conditions, is growing. A recent NHS Confederation publication has suggested that by 2050 spending on obesity will rise to £9.7bn per year and malnutrition will cost the NHS £19.6bn per year³. With such a staggering impact, food and drink will, no doubt, play a crucial role in an ICS’ strategy for improving their population health outcomes and healthcare provision.
However, there is a growing body of evidence that demonstrates the impact malnutrition and dehydration can have on shorter term patient outcomes. The ‘Guidance – Commissioning Excellent Nutrition and Hydration’⁴ highlights the consequence for hospital stays; patients average an additional 3 days’ length of stay, with delayed and failed discharges and increased complications being commonplace.
However, despite the increased focus, malnutrition of patients remains a challenge for hospital inpatients as 60% of patients continue to face a decline in nutritional status following admission.⁵
The relationship between inpatient experience and hunger
There are several areas which could positively impact the growing nutrition and hydration challenge, and patient experience is a core component of many of them. Having a positive hospital experience directly impacts the speed of recovery, and food plays a key part in this according to patients.
A recent YouGov/Sodexo survey⁶ found that 93% of people believe that they are more likely to get better quicker and leave hospital sooner if they had a positive hospital experience. Furthermore, one third of inpatients cited the quality and availability of food and drink as a key factor contributing to their overall experience⁶.
In 2008, research⁷ exploring inpatients’ experience of access to food found that most patients were satisfied with the meals they received while in hospital, however almost half felt hungry during their stay because of difficulties accessing food. It was often cited that availability of food after admission, between mealtimes and after treatment were causes of hunger.
The most recent CQC adult inpatient survey found that the overall experience of inpatient care has fallen in recent years from 56% in 2020 to 52% in 2021⁸. As the overall experience worsens, the challenge of ensuring patients are well fed increases.
Reducing the impact food and drink has on the environment
As well as considering governance, quality and choice, the new National Standards also recognise the role hospital food and drink has on achieving the NHS’ aim to be net zero by 2045⁹. The management of the facilities services plays a crucial role in achieving this – currently contributing 15% of the total carbon emissions.¹⁰
Monitoring food waste and determining actions to minimise production and plate waste will become an estates and facilities reporting requirement in the coming year. So, not only do providers have a challenge of enhancing quality, choice and experience, they must do so while reducing the impact delivering these services have on the environment.
Assessing the challenges in the end-to-end journey
Recognising the impact food and drink has on a patient’s recovery, and having helped inform the National Food and Drink standards, Sodexo Health & Care undertook an 18-month programme to determine where access and experience could be enhanced during the patient journey.
Conducting extensive patient and clinical staff research identify the challenges and barriers faced - uncovering potential solutions to enhance the offer for patients, staff and visitors.
The programme found that five key factors have the biggest impact on patient and staff hydration and nutrition:
- Understanding the local challenges patients and staff face – each site will be different
- Facilitating greater knowledge of where/when food and drink can be obtained - better, consistent communication
- Enhancing the availability times and locations of food and drink – increasing access
- Increasing capacity through quasi-clinical tasks – freeing clinicians’ time for other tasks
- Considering the full journey – beyond inpatient dining.
The research uncovered several challenges faced during the patient’s recovery journey which, if addressed, could significantly enhance the food and drink experience and therefore hydration and nutrition levels. However, new ways of thinking would be required to move away from the status quo.
Recovery journey challenges and solutions
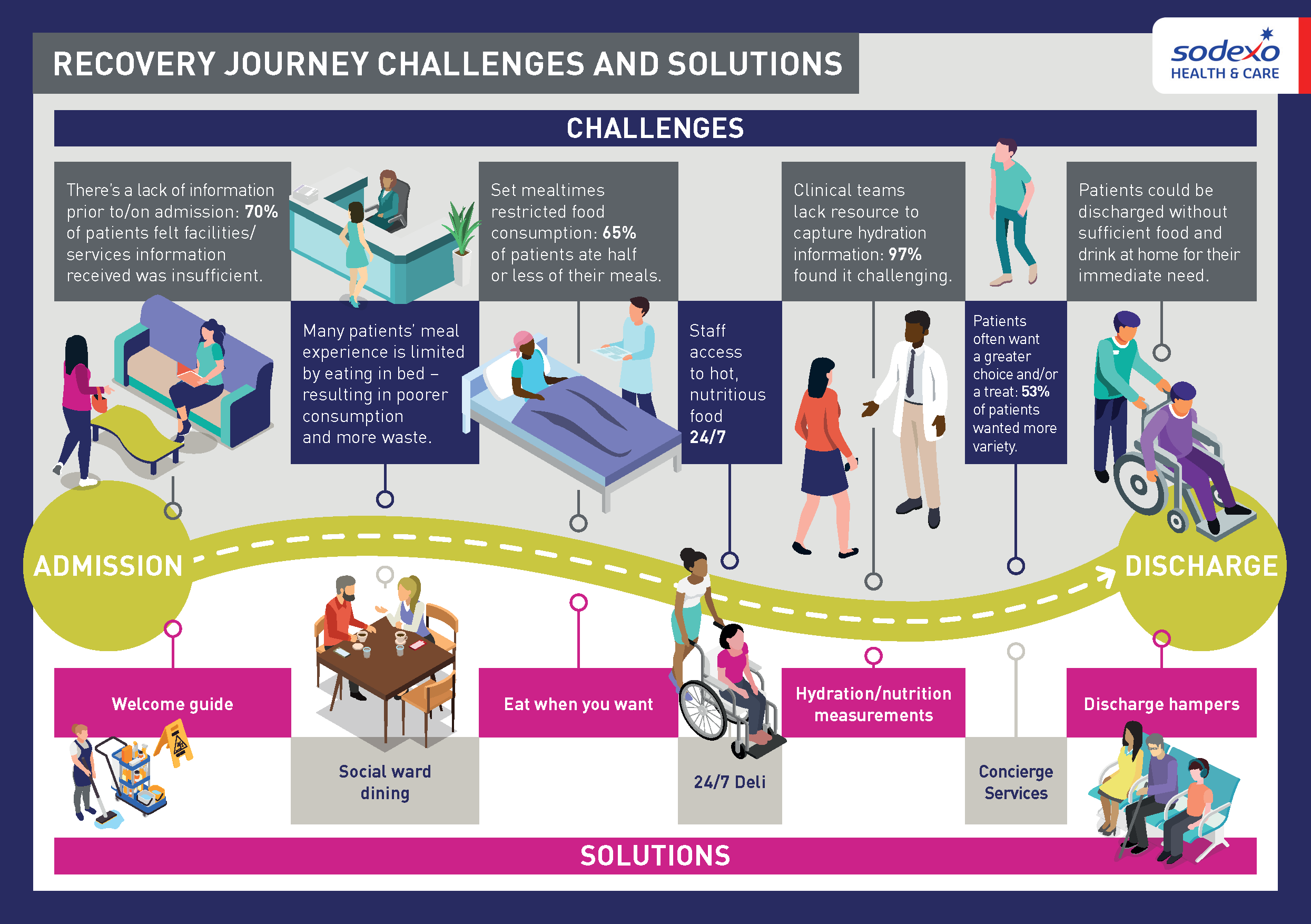
Solutions to address the challenges
During the patient journey programme, Sodexo identified, piloted and now have solutions to address the challenges patients and clinical teams were facing.
Below provides a flavour of some of the innovations now available.
Welcome Guide
Through the research, Sodexo discovered that a lack of information on admission impacts the patient experience from the outset and throughout. Patients felt that limited access to information resulted in uncertainty and a loss of control over their experience.
70% of patients felt that they had insufficient information about their hospital visit prior to admission and on arrival (including facilities and services available).
Sodexo developed, and piloted with a partner NHS Trust, a Digital Welcome Guide which provides a range of information, empowering patients at their point of admission by providing information on patient dining menus, who’s who in the team, hospital and ward routines, FAQs and ways to feedback.
The impact on the patient experience was significant:
- All patients surveyed who accessed the Welcome Guide said it significantly enhanced their patient experience
- 91% of patients needed to ask fewer questions as they had the information to hand.
The Digital Welcome Guide not only enhanced the patient experience, it also gave time back to clinical teams for more patient-centric tasks:
- 80% of the clinical team believed they spend over 30 minutes a day answering non-clinical information questions from patients.
Flexible eating solution
Since the inception of the NHS, delivery and mealtimes of patient dining has remained almost unchanged, despite the developments in our eating habits and expectations. This gap was identified as one of the major challenges in supporting a patient’s hydration and nutrition:
- Only 26% of patients ate all or most of their meal – many suggested choice and timing of the meal service was the reason
- 70% of patients felt that having a more flexible solution would significantly enhance their experience.
Sodexo implemented a flexible eating solution where patients could call for a ward host to order food, from a menu placed by their bedside, from 7.30am-9.30pm. The ward host was aware of any specific patient dietary/allergen requirements, which were captured in our electronic food ordering solution. Meal preparation, safety and delivery all followed our standard procedures – ensuring compliance and governance were maintained throughout.
Food consumption, nutritional balance and overall satisfaction significantly increased:
- 78% of patients ate all or most of their meal with flexible eating – compared to 26% on the standard model
- Only 1% of patients didn’t consume any protein, vegetables or carbohydrates – compared to 8% previously
- 96% of patients would recommend that other hospitals/wards introduce this solution.
I was looking at the work Sodexo are doing around flexible eating. We need to understand that if you’re more adaptable around your timings, and food choice, then people will eat better and recover quicker. It’s a great initiative.”
Phil Shelley, Chair of the National Food Review
Hydration and nutrition measurements
Clinical teams also struggle to capture hydration and nutrition data used to inform patient care plans:
- 97% of staff found it challenging to capture this data alongside other clinical roles
- 91% believe that having another team undertake non-clinical tasks frees up their time and enhances clinical efficiency.
It was also identified that supporting patient hydration and nutrition was not the responsibility of one individual or team. Collaborative working, breaking down silos, would be essential to make tangible improvements.
Sodexo undertook a programme to capture information of patients’ hydration and nutrition consumption, while at the same time measuring waste, presenting the data back to the clinical team to help inform treatment and care plans.
As well as being able to capture the data more frequently (67%), the clinical teams cited several benefits of a support team capturing this information:
- 72% frees up time for other clinical tasks
- 49% more accurate information.
Concierge services
When patients’ length of stay is significant, or they have limited mobility, choice and variety becomes an even greater factor in their nutrition and hydration. During the programme, the research discovered that many patients wanted a greater choice of food (53%) or even just something which provided a treat to make them feel better (57%) on our long-stay spinal injury wards.
Sodexo introduced a Concierge service, which provided a dedicated team member to order and collect food on their behalf – within and from outside of the hospital. This could range from supermarket groceries to something as simple as a Friday night take-away.
- Patients rated the Concierge Service 4.95/5
- All patients felt their experience was enhance by the Concierge Service.
For more information about these new, exciting initiatives, plus other developments to enhance the wellbeing of patients, visitors and staff, speak with us today.